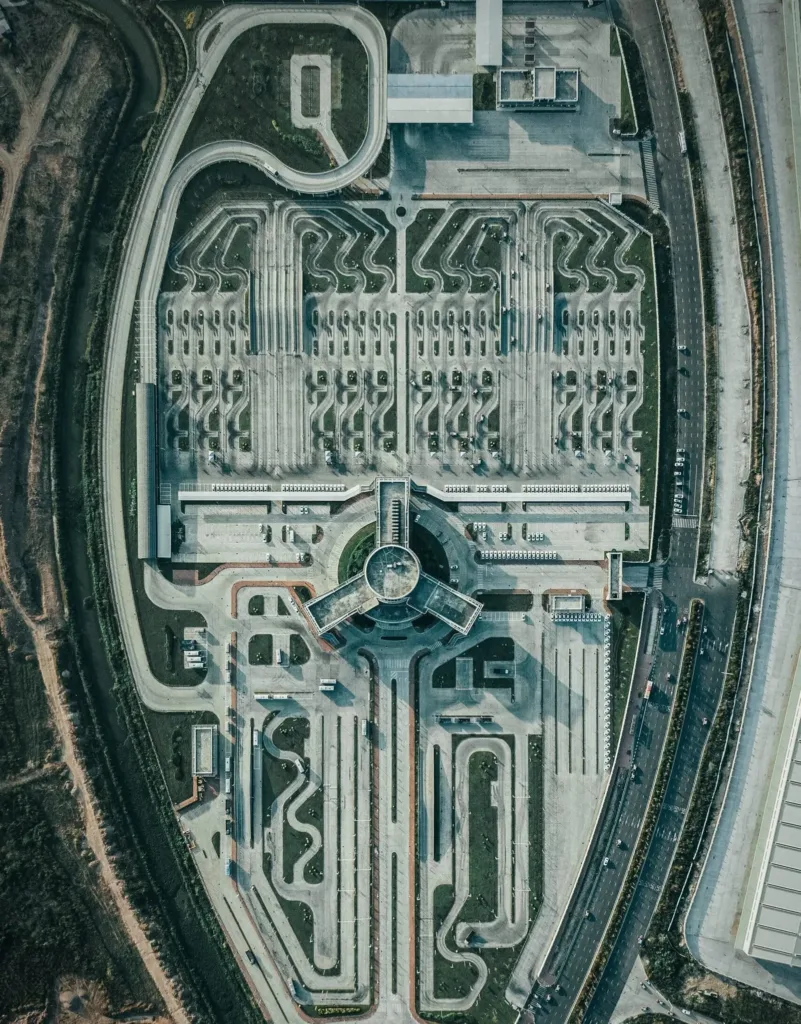
This whitepaper explores how end-to-end process automation and cross-functional orchestration can help insurers and medical schemes evolve from rigid service providers to adaptive, scalable, and customer-centric platforms — while preserving compliance and cost control.
1. A Sector Built on Complexity — and Broken by Fragmentation
Medical insurers process thousands of real-time activities across disparate systems and touchpoints:
- Claims submission, validation, and payment
- Member onboarding and plan changes
- Provider credentialing and payment processing
- Pre-authorisations and case management
- Fraud detection and audit trails
- Regulatory submissions and scheme reporting
Most insurers and medical schemes operate on a legacy patchwork of platforms (e.g., AS/400, Oracle Health Insurance, TCS BaNCS, custom claims engines) with manual workarounds and disconnected workflows across business, IT, legal, and clinical teams.
The result is often:
- Delayed claims processing and member service
- Duplicate tasks and rework
- Compliance gaps and audit fatigue
- Unsustainable staff workloads
- High operational costs and error rates
2. Automation vs Orchestration — and Why Both Are Needed
- Automation eliminates manual tasks (e.g., straight-through claims processing, KYC checks, bulk communications).
- Orchestration aligns end-to-end workflows across teams, systems, and rules — handling approvals, exceptions, escalations, and data dependencies.
In medical aid and insurance, orchestration is critical because workflows are:
- Non-linear (e.g. a claim may trigger pre-authorisation, audit, or fraud alert)
- Highly regulated (e.g. privacy, payment timelines, patient rights)
- Multi-party (e.g. member, scheme, provider, broker, regulator)
- Exception-heavy (e.g. special billing codes, pending documents, plan changes)
Without orchestration, automation becomes isolated — and systemic inefficiencies persist.
3. Key Use Cases for Automation and Orchestration
- a) End-to-End Claims Processing
- Auto-validation of codes, limits, and eligibility
- Rules-based routing to human adjudication only when needed
- Seamless escalation to fraud or case review
- Auto-generated communications and remittance
- b) Member Lifecycle Management
- Trigger-based onboarding workflows (KYC, policy docs, card issuing)
- Auto-handling of plan upgrades, terminations, and benefit changes
- Integration with CRM, billing, and compliance systems
- c) Provider Management and Payments
- Credentialing orchestration with real-time verification
- Automated handling of payment cycles, rejections, and reconciliation
- Rules-driven resolution of tariff exceptions or clawbacks
- d) Pre-authorisation and Clinical Review
- Automated workflow for benefit checks, clinical rules, and approvals
- Orchestration of referrals to doctors, case managers, or second opinion panels
- e) Compliance and Reporting
- Sequenced workflows for data sourcing, validation, signoff, and audit trail
- Real-time readiness for regulators (e.g., solvency, claims ratios, consumer protection)
4. Strategic Benefits
|
Objective |
How Automation & Orchestration Help |
|
Improve Customer Experience |
Faster claims, fewer errors, self-service capabilities |
|
Boost Operational Efficiency |
Lower manual workloads, better resource allocation |
|
Enhance Compliance |
Enforce rules and audit trails systematically |
|
Reduce Risk |
Prevent revenue leakage, detect fraud, flag exceptions early |
|
Accelerate Change |
Add new plans, rules, or products without disrupting core systems |
|
Enable Scalability |
Handle more members or providers without proportional cost increases |
5. Implementation Approach: Orchestration as an Operating Model Shift
At Tidus, we advocate treating automation and orchestration not just as IT upgrades, but as operational redesign initiatives. Our proven approach includes:
- Process Mapping and Failure Point Analysis
- Orchestration Flow Design – Events, triggers, business rules, exceptions
- Integration with Core Systems – EHRs, CRM, billing, document stores
- Governance Layer Design – Approvals, escalation, audit visibility
- Analytics-Driven Optimisation – Identifying lag, bottlenecks, and cost drivers
We apply Operations Research principles to optimise flows, and ensure automation adds real business value, not just cosmetic speed.
6. Real Example Scenarios
|
Scenario |
Without Orchestration |
With Orchestration |
|
Claim requiring additional documents |
Back-and-forth emails, delays, manual flags |
Workflow triggers document request, pauses claim, alerts member, auto-resumes |
|
Member changes plan mid-cycle |
Manual updates across systems, error risk |
Workflow validates eligibility, updates all systems, recalculates premiums |
|
Provider audit trigger |
Missed deadlines, untracked escalations |
Auto-routing to audit team, flagged in dashboard, prepopulated data review |
Conclusion: From Bottlenecked to Borderless
In a sector where speed, trust, and compliance matter equally, automation and orchestration are no longer optional. They are the foundation for sustainable, adaptive, and customer-focused insurance operations.
Firms that invest in these capabilities now will unlock lower costs, higher member retention, and next-generation agility — gaining a clear edge in a competitive and heavily regulated environment.
Tidus helps insurers and medical aid schemes bridge the gap from rigid process to orchestrated performance — combining automation with engineered operations.